Technology Innovations Transforming Healthcare in 2025 are reshaping how care is accessed, diagnosed, and experienced by patients, driven by the convergence of artificial intelligence, high-speed connectivity, advanced devices, and data-driven workflows that empower teams to act sooner, personalize plans, and enhance safety in both hospital settings and at home. Across clinics, labs, and community hubs, AI in healthcare 2025 is powering diagnostics, risk stratification, triage, and predictive alerts that augment, rather than replace, clinicians’ expertise, helping to flag subtle patterns in imaging, genomics, and longitudinal records, while respecting patient preferences and maintaining human-centered decision-making. Telemedicine expansion and remote patient monitoring extend care beyond the clinic walls, improving access for rural and underserved populations, enabling timely interventions for chronic conditions, supporting care continuity during emergencies, while reducing travel burdens, lowering costs, and strengthening the patient’s sense of control, a shift that is catalyzing new care delivery models, reimbursement pathways, and the normalization of virtual consultations as a standard option. Wearable health tech and continuous monitoring provide longitudinal signals—from heart rate and sleep to glucose trends and activity—feeding secure cloud records that clinicians can interpret to tailor interventions, support behavior modification, and empower patients to participate actively in decision-making while maintaining privacy and data integrity. From robotic-assisted surgery to precision medicine and interoperable data ecosystems, these innovations are elevating safety, efficiency, and patient-centered outcomes across diverse health systems, while challenging clinicians to adapt workflows and payers to align incentives with higher-value care.
Another way to frame these developments is through digital health breakthroughs, intelligent clinical systems, and data-enabled care pathways that recast the patient journey. Rather than focusing on isolated devices, the emphasis shifts to smart analytics, adaptive imaging, genomics-guided therapies, and decision-support ecosystems that tailor treatments to individual biology. Remote care networks, wearable sensors, and virtual visits are reshaping screening, treatment initiation, and recovery, while interoperable data platforms and strong governance underpin trust, privacy, and scalable adoption. In the operating room, robotic-enabled procedures, image-guided surgery, and automated workflows illustrate how capability, precision, and efficiency converge to improve outcomes. Equity, safety, and ethical considerations remain central to translating these trends into real-world value for diverse populations.
Technology Innovations Transforming Healthcare in 2025: AI, Telemedicine, and Precision Medicine in Action
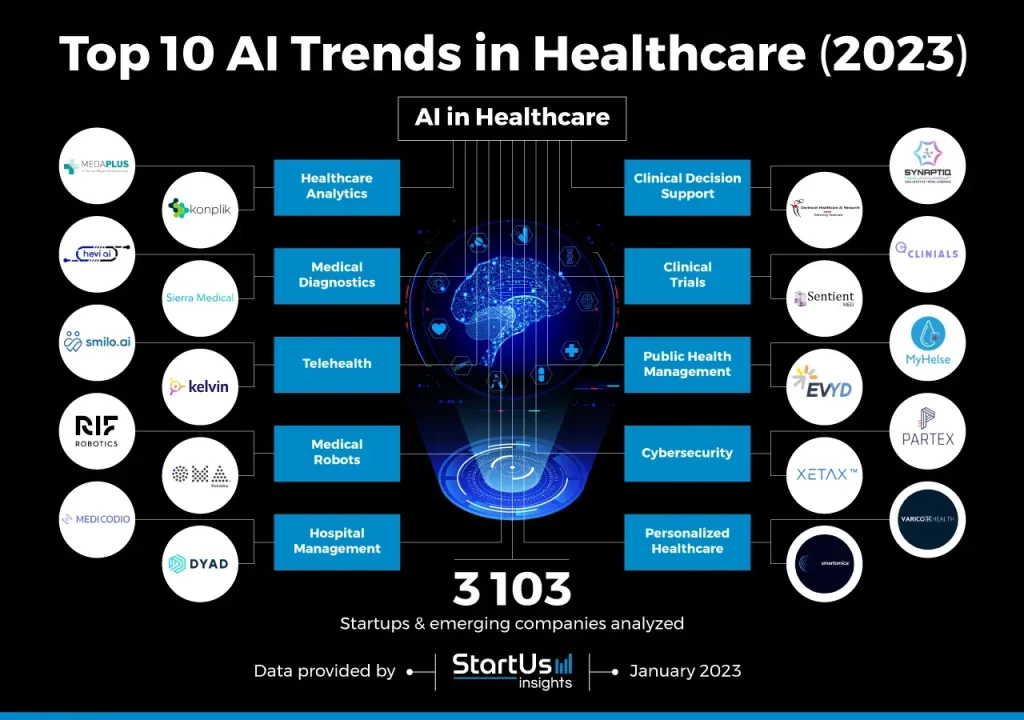
AI-driven diagnostics and predictive analytics are reshaping how clinicians interpret data. In 2025, AI in healthcare 2025 is applied to imaging, genomics, and electronic health records to provide decision support, risk stratification, and early warning signals. When combined with clinician expertise and patient preferences, these insights enable earlier interventions, more accurate diagnoses, and a stronger shift toward value-based care.
Beyond the patient encounter, a robust digital infrastructure—interoperable EHRs, cloud-based data platforms, and standardized interfaces—underpins the promise of Technology Innovations Transforming Healthcare in 2025. Precision medicine comes alive as omics data, pharmacogenomics, and personalized treatment plans are guided by secure analytics and seamless data sharing. Yet success relies on data governance, privacy protections, and ensuring equitable access so that advanced capabilities improve outcomes for diverse populations.
Wearable Health Tech, Robotic-Assisted Surgery, and the Future of Patient-Centered Care
Wearable health tech and continuous monitoring turn everyday devices into proactive health partners. Smartwatches and biosensors capture metrics like heart rate, activity, and sleep, enabling early detection, behavior modification, and population health insights. When these data streams feed into clinician dashboards and telemedicine-enabled care teams, providers can intervene sooner, adjust therapies in real time, and support remote patients with confidence.
Robotic-assisted surgery marks a mature frontier for precision and safety in the operating room. Advanced robotic platforms enhance visualization, precision, and control, enabling less invasive procedures with faster recoveries and fewer complications for suitable cases. The broader impact extends into automation of hospital workflows and AI-guided planning with augmented reality overlays, illustrating how Technology Innovations Transforming Healthcare in 2025 translate into tangible improvements for patients and care teams.
Frequently Asked Questions
How is AI in healthcare 2025 shaping diagnostic accuracy and care delivery as part of Technology Innovations Transforming Healthcare in 2025?
AI in healthcare 2025 enhances diagnostics by rapidly analyzing imaging, genomics, and EHR data, enabling earlier detection, risk stratification, and supports precision medicine decisions. When combined with clinician expertise and patient preferences, AI provides actionable insights that support targeted treatments and value-based care, a core element of Technology Innovations Transforming Healthcare in 2025.
How do telemedicine expansion and wearable health tech illustrate Technology Innovations Transforming Healthcare in 2025 for patients and providers?
Telemedicine expansion and wearable health tech extend access, enable continuous remote monitoring, and empower patients to participate actively in their care. By delivering real-time data into clinical workflows, these tools support proactive management, improve outcomes, and embody the patient-centered focus of Technology Innovations Transforming Healthcare in 2025.
| Key Topic | Summary | Impact on Stakeholders | Notes / Examples |
|---|---|---|---|
| AI-driven diagnostics and predictive analytics | AI interprets imaging, genomics, and EHR data at speed to support decision making, risk stratification, and early warnings. When combined with clinician expertise and patient preferences, it enables more precise, timely diagnoses and moves toward value‑based care. | Clinicians, patients, payers, researchers; faster diagnoses; improved outcomes; potential cost savings. | AI-identified patterns can flag risks (e.g., sepsis, heart failure); effectiveness depends on data quality and integration with clinical judgment. |
| Telemedicine expansion and remote patient monitoring | Platforms enable care beyond clinics; continuous remote monitoring improves access, reduces travel burden, and supports chronic disease management with real-time or near real‑time data. | Patients (especially in rural areas), clinicians, health systems, payers; improves access and potentially reduces costs. | Core component of modern primary care; supports regular check-ins and proactive management. |
| Wearable health tech and continuous monitoring | Wearables provide longitudinal data on heart rate, activity, sleep, and more; enable early detection, behavior change, and population health management; cloud integration with clinical records; AI-assisted interpretation. | Clinicians, patients, population health initiatives; improved trend monitoring and personalization. | Validated for clinical use; AI aids interpretation and ties data to care decisions. |
| Robotic-assisted surgery and automation in the OR | Robotics improve visualization, precision, and control for less invasive procedures; faster recovery and fewer complications; automation enhances hospital workflows (sterile processing, logistics). | Surgeons, patients, OR staff, hospital operations teams; overall care efficiency and outcomes. | Integration with imaging, AI planning, and augmented reality supports complex tasks with higher confidence. |
| Precision medicine and genomics | Personalized treatments based on genetics, environment, and lifestyle; sequencing, targeted therapies, and pharmacogenomics guide decisions; secure data sharing and cross-disciplinary collaboration are required. | Patients, clinicians, researchers, and drug developers; improved targeting and potentially better outcomes. | AI-enabled omics analysis informs risk assessment, treatment selection, and monitoring. |
| Digital health records, interoperability, and data clouds | Cloud platforms, standardized interfaces, and privacy controls enable accessible, interoperable data across settings; reduces duplication and accelerates research; emphasizes data governance. | Clinicians, researchers, payers, and patients; smoother care coordination and faster insights. | Secure governance is critical as data volumes grow; interoperability reduces silos. |
| Digital twins, simulation, and clinical trials | Digital twins simulate patient-specific anatomy or treatment responses for risk‑free planning; virtual trials accelerate development and reduce costs. | Researchers, developers, patients; faster, cheaper trial design and iteration. | Integration with AI and real‑world data enables faster translation from concept to bedside. |
| Augmented reality (AR) in training and planning | AR overlays provide real-time, context-aware guidance during procedures and education; enhances training and remote mentoring. | Trainees, clinicians, OR teams; improved precision and learning outcomes. | AR visualizes anatomy and device placement to support decision making. |
| Privacy, security, and ethical considerations | Safeguard privacy and security with encryption, access controls, and governance; address bias, equity, and informed consent; establish standards. | Patients, providers, regulators, and society; trust and safety are foundational. | Ongoing governance and standards development are essential to balance innovation with protection. |
Summary
Technology Innovations Transforming Healthcare in 2025